Spotting the signs of coeliac disease or gluten intolerance can be a long and arduous affair – Michelle Kickham explains the differences and what to look out for…

Ah, gluten. It puts the spring in our cakes, the stretch in our dough and much to our dismay, is often found in those feel-good foods. However, sometimes the cure is worse than the disease as gluten is one of the most common causes of digestive and autoimmune disorders. With the increasing number of digestive disorders being discovered it can be difficult to know whether you suffer from coeliac disease, you have an allergy or if you are gluten intolerant; something that becomes very important when it comes to diagnosis and treatment options.
What is gluten intolerance?
It’s difficult to pinpoint exactly what gluten intolerance is as there is no known cause or biomarker (a biological signature for a disease) for this condition. It typically presents with symptoms similar to coeliac disease including bloating, cramps, memory dysfunction or ‘brain fog’ and diarrhoea, but lacks the immune response seen in coeliac disease and food allergies.
What causes it?
There is no known cause of gluten intolerance, although research suggests that it may be due to a mixture of genetics, nationality and just bad luck! Gluten is also rich in the amino acid Proline, which is difficult for the body to break down when compared to other amino acids, meaning those with a ‘lazy digestive system’ may be more predisposed to suffer with it. Despite the lack of understanding of this condition, it is nonetheless important to take action in order to prevent potential side effects such as weight loss, dehydration and cognitive decline.

Coeliac disease vs gluten intolerance
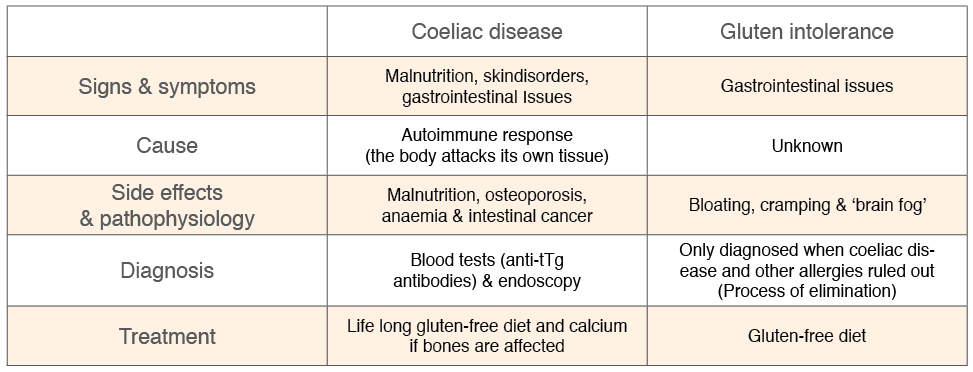
Although gluten intolerance, coeliac disease and wheat allergies all share some common symptoms, they are in fact all very different disorders. Wheat allergies are easily explained – you’re allergic to wheat. Bummer, but easily treated! The other two though, they’re complicated – as you’ll soon see.
Coeliac disease is an autoimmune disease – not an intolerance, allergy, or dietary choice (despite the recent ‘gluten-free!’ fad). An auto-immune disease is when the body attacks its own cells, either through antibodies or T-cells, leading to atrophy of tissue (organ damage), inflammation and in some extreme cases, death. In coeliac disease, the body sees gluten as a ‘danger’ and mounts an immune response by producing specific antibodies (small molecules which bind to and help rid the body of dangerous invaders such as bacteria and fungi) against it. These antibodies not only attack the gluten, but also our small intestine which (trust me!) is not exactly a pleasant experience. If left untreated, coeliac disease can lead to serious health conditions such as malnutrition, osteoporosis and even colon cancer.
In contrast, non-coeliac gluten intolerance does not result in the production of antibodies or any immune response. There are no specific blood markers to signify gluten intolerance is present and almost all cases of gluten intolerance are based on anecdotal evidence such as the physical symptoms listed above. Despite the lack of diagnostic markers, it is indeed recognised as a digestive disorder and requires medical attention and appropriate treatment.

Diagnosis – which is it?
As already explained, there is no definitive biomarker known with the ability to diagnose non-coeliac gluten intolerance. As such, diagnosis of gluten intolerance relies on the process of elimination of coeliac disease and any other food allergy.
Diagnosis of coeliac disease begins with a simple blood test where they check for the presence of anti-tTg antibodies (the nasty antibodies mentioned above that declare war on your tummy) and two other antibodies (IgA and IgA EMA) which are known to be elevated in cases of coeliac disease. If blood tests confirm the presence of these dangerous antibodies, an endoscopy and intestinal biopsy (a lovely experience!) is commonly performed to finalise the diagnosis.
Diagnosis of non-coeliac gluten sensitivity only occurs when coeliac disease and other food allergies (such as wheat and dairy) are ruled out. Basically, the diagnostic process for each condition is the same, the only thing that differs is the result. It might surprise you to hear that coeliac disease actually only affects about 1% of the population, and in most cases diagnosis falls within the food allergy or intolerance area.
Treatment and action plan
Whether you are diagnosed with coeliac disease or gluten intolerance, treatment for each is essentially the same; remove all sources of gluten from your diet. Sounds easy, but once you are told to avoid it, you’ll notice that it tends to pop up in the strangest places – even diet cola drinks!
Transitioning to a gluten-free diet for life can be a bit daunting, so be sure to check in with a nutritionist or do your own research by availing of many online resources. It is very important to stick to your diet, as a simple slip-up can have devastating effects.
Sure, the French baguette looks good now, but come to me an hour later and you’ll be seriously questioning your decision making!